Seriously, stop it.
For many people the first choice when their shoulder begins to hurt or if they lack mobility is to start cranking and yanking on it. This is rarely the right approach, and as Andrew Millett (my good friend and Boston based physical therapist) points out in today’s post…there a far better and far more effective approaches.
Enjoy.
Copyright: staras / 123RF Stock Photo
The shoulders, specifically, the glenohumeral joints, are typically very mobile joints. They need to flex, extend, abduct, adduct, horizontally abduct and adduct and internally and externally rotate in multiple planes and positions in relation to the body. Even though the shoulders are a common area of mobility, many people will present with limitations in at least one aspect of glenohumeral motion.
There are various reasons why someone may have limited shoulder mobility.
Bony Limitations
photo credit: pediatric-orthopedics.com
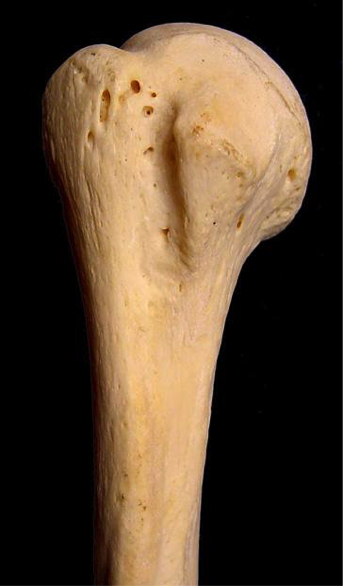
People who engaged in various overhead sports such as baseball, softball, etc. have been shown on multiple studies to have changes to the glenoid and humeral head. In baseball players specifically, they can appear to have a loss of internal rotation range of motion as compared to their non-throwing shoulder and an increase in external rotation range of motion as compared to their non-throwing shoulder.
This change in range of motion is commonly due to humeral retroversion. Humeral retroversion is the alternation of the humerus and humeral head in relation to the glenoid fossa from years of repetitive overhead activity, specifically throwing.
Photo credit: opensiuc.lib.siu.edu
This is typically only seen in overhead athletes. This differentiation in range of motion side to side in external and internal rotation is considered “normal” for this population. As long as External + Internal Rotation aka Total Motion is within 5 degrees of the non-involved shoulder, then that is considered normal.
Note from TG: In other words, loss of IR in a throwing shoulder is an adaptive response and is normal! It doesn’t necessarily have to be fixed.
With that said, we do not want to crank on someone who has “normal” total motion, but may lack internal rotation on one side versus the other. Asking your patient or client if they engaged in overhead sports as a child is a good clue to this. Then measuring their motion will give more information.
We will get into more detail later on how to improve their motion if their is more than a 5 degree difference in total motion.
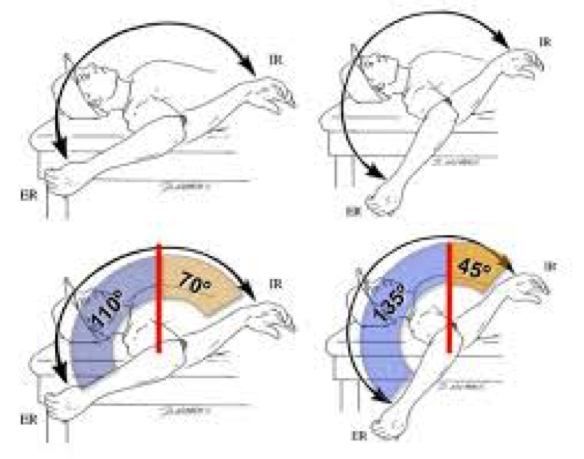
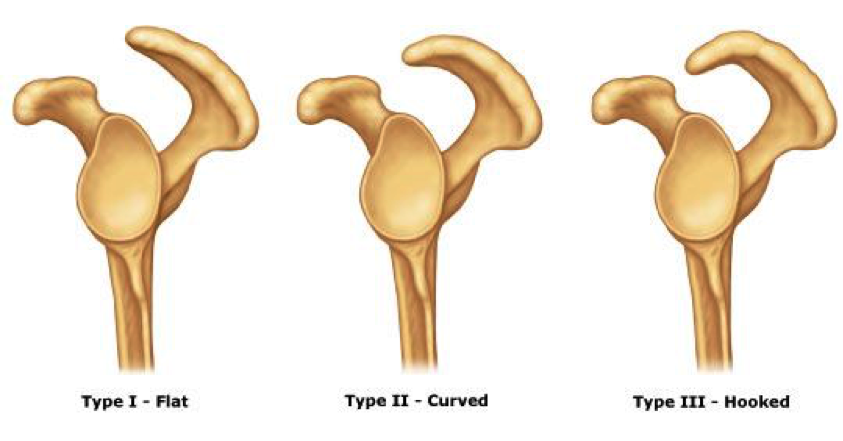
Another bony limitation at the shoulder can be acromion type. The acromion is a bony structure that is present in all people that is part of the scapula.
Photo credit: ipushweight.com
All acromions are not created equal though. There can be 3 varying types of acromions.
Photo credit: cursoenarm.net
As you can see in the picture above, a type I acromion is relatively normal in appearance. In type II and III, there is more of a curved/hooked appearance to it. This alteration in can cause pain and limited motion when reaching overhead.
The only way to definitively know if someone has a type II or III acromion is through radiographic imaging. Programming may need to be altered to more horizontal pulling/pushing variations instead of overhead work if someone doesn’t have full overhead mobility due to a type III acromion.
For most people with a type II acromion, physical therapy can help to improve range of motion and decrease the effect of the acromion on shoulder motion and pain. For most people with a type III acromion, more often than not, surgical intervention is what will help.
Capsular Limitations
In the majority of the joints in the body, there is something called a “capsule” surrounding the joint. A capsule is synonymous to a ziploc bag encompassing the joint.
In this capsule, there are “folds” in certain aspects depending on where the arm is positioned. Due to an old injury, surgery, etc., this capsule can become “tight or stiff.” Now, without getting into too much detail about why it is tight/stiff or why there are capsular limitations, the only way to determine if there is capsular limitations, is by a licensed healthcare practitioner, ie. PT, chiropractor, etc.
Typically, older populations may have more capsular limitations OR if someone has had a long standing injury or prior surgery to the shoulder, they may present with decreased ranges of motion because of the capsule.
The only other area that can be attributed to decreased ranges of motion due to the joint capsule itself that affects the shoulder, would be the thoracic spine. Lack of thoracic spine extension and/or rotation can limit shoulder flexion, external rotation, etc.
To test for limited thoracic spine mobility, try Quadruped Passive Thoracic Rotation:
Normally, passive rotation should be 50 degrees in the general population. If it is less than that, that can significantly limit shoulder range of motion.
Soft Tissue Restrictions
Now, this is the more common of all three of the factors that can limit shoulder mobility. Excluding clients who are hyper-mobile, the majority of clients and patients have some form of increased soft tissue tone in one if not more areas of their body.
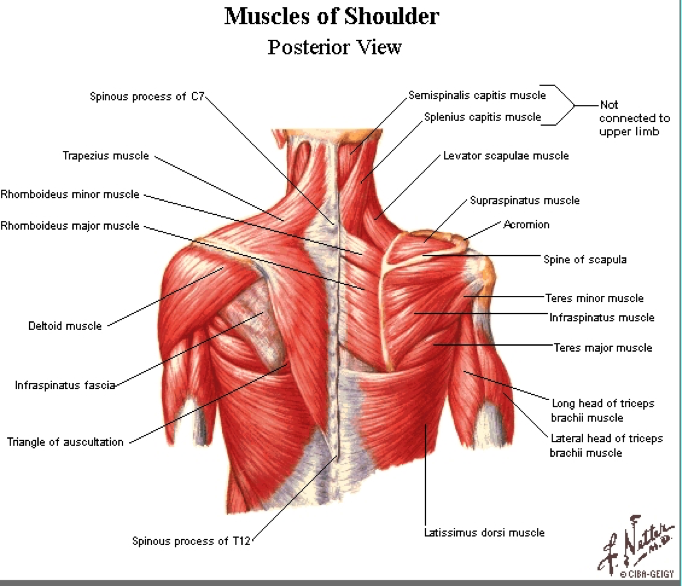
At the glenohumeral joint, there are a few “big” than can contribute to limited shoulder mobility.
Photo credit: www.smogshoulder.com
Muscles that can limit shoulder flexion are:
- Pectoralis Major/Minor
- Teres Major
- Latissimus Dorsi
- Subscapularis
Muscles that can limit shoulder abduction are:
- Pec Major/Minor
- Teres Major
- Latissimus Dorsi
- Subscapularis
Muscles that can limit shoulder external rotation are:
- Pec Minor
- Teres Major
- Latissimus Dorsi
- Subscapularis
Muscles that can limit shoulder internal rotation are:
- Infraspinatus
- Teres Minor
Now, you’re probably thinking that I just “copied and pasted” most of those muscles from one section to the other. The latissimus dorsi is a huge contributor to limited overhead shoulder mobility due to its attachment on the trunk into abduction and flexion. It can also limit external rotation as it is a shoulder internal rotator.
Pectoralis minor can limit overhead motion because of its attachment on the coracoid process of the scapula and the rib. Decreased pectoralis minor tissue extensibility can cause an anterior tilt of the scapula limiting humeral motion on the glenoid.
Subscapularis can limit overhead motion due to its attachment on anterior side of the scapula and on the humerus. Teres major attaches on the scapula as well as on the humerus and can limit overhead mobility as well.
Infraspinatus and Teres Minor limit internal rotation of the shoulder due to its attachment points on the humerus and scapula.
Typically, one if not more than one of the aforementioned muscles can limit overhead mobility. Instead of performing intense stretches and forcing the glenohumeral joint into motions it just does not have, we need to ASSESS and then ADDRESS any limitations that are present.
Assessment
Active Motion
To assess someone’s active ranges of motion, ask them to move.
Have them perform:
Shoulder Flexion
Shoulder Abduction
Shoulder Medial Rotation
Shoulder Lateral Rotation
“Normal” ranges of motion for general population clients would be:
Shoulder Flexion: 180 degrees OR humerus in line with the client’s ear.
Shoulder Abduction: 180 degrees OR humerus in line with side of body
MRE: 3rd digit finger tip to contralateral inferior angle of scapula
LRF: 3rd digit finger tip to superomedial border of contralateral scapula.
Now that you have assessed someone’s active motion, we need to assess it passively to fully determine if someone has a true mobility limitation.
Passive Motion
Perform the same motions passively into flexion, abduction, MRE, and LRF. Do not force these motions or push through tightness or pain. If you cannot passively bring the client’s arm to the aforementioned areas mentioned in the Active Motion section, then we know the client has a true mobility limitation.
Addressing the Issue
If someone presents with limitations in passive shoulder flexion, abduction, MRE, or LRF, performing some form of Self-Myofascial Release (SMR) can be beneficial.
Then, re-test passive motion to see if there has been an improvement in mobility. If there has, then you know you have worked on the appropriate areas.
If there has NOT been an improvement in mobility, refer out to a manual therapist (PT, sports chiropractor, massage therapist, etc.)
If the mobility has improved, then we want to use appropriate mobility drills to help groove the patterns that were just improved.
Horizontal Adduction/Posterior Rotator Cuff Stretch
Key Points:
- Make sure to keep scapulae retracted by using wall or door jam.
- Once scapulae is fixed, gently bring arm across body.
- Hold 5-8 seconds pre-training or 30 seconds post-training.
- By fixating scapulae, it will provide a more focused stretch to the posterior aspect of the shoulder.
Latissimus Dorsi Stretch
Key Points:
- Use opposite side hand to fix scapulae to rib cage.
- Once scapulae is fixed, hold onto a stationary object and sit back.
- Gentle stretch should be felt in the lat.
- By fixating the scapulae to the rib cage using the opposite hand, it provides a truer stretch to the lat vs tractioning the glenohumeral joint.
Motor Control
Once there has been an improvement in mobility, we want to make sure that the brain and the body knows how to access that “new” mobility. We need to make sure to re-pattern the proper movement patterns to avoid falling back into an poor compensations.
For shoulder re-patterning, various movements that help to promote proper movement patterns such as:
Forearm Wall Slides
Back to Wall Shoulder Flexion
Quadruped Assisted Reach, Roll, and Lift
Now that we have improved the mobility by addressing increased soft tissue tone, re-patterned those movement patterns, now we want to incorporate them all together.
Movements such as:
Turkish Get-Up
Kettlebell Bottoms Up Baby Get-Up
There you have it! Instead of mindlessly stretching your shoulder, address any potential limitations and get back to training effectively!
About the Author
Andrew Millett is a Metro-West (Boston) based physical therapist
Facebook: From The Ground Up
Twitter: @andrewmillettpt