You all know the stat: upwards of 80% of the population will experience some form of debilitating back pain – often times a disc herniation – in his or her’s lifetime.
It can strike with one dubious rep on a set of deadlifts, bending over to pick up a child, or, I don’t know, during a random after hours office Fight Club.
However (0r whenever) it happens, it sucks. But what also sucks is the often archaic advice many receive with regards to what to do when a disc herniation happens.
In today’s guest post by UK based physical therapist and strength coach Alex Kraszewski, he helps to set the record straight.
Enjoy.

Why You Can and Should Lift Weights With a Herniated Disc
Just like Crossfitters, Vegans and Anti-Vaxxers1, if someone has back pain and they think it’s a disc herniation, it’s probably the first thing they’ll tell you.
There’s not many days that go by where I don’t see someone with back pain, and in more cases than I’d like – the opening conversation tends to go like this;
Me: “So what brings you in today and how can I help you?”
Client: “My doctor/chiro/shamanic healer said I’ve got a disc out, a trapped nerve and my MRI proves it. It hurts and I need you to put it back in.”
Me:
The intervertebral disc has become the scapegoat for a lot of back pain and disability. When the word ‘disc’ is used, it tends to create a cascade of fear, anxiety and worry for the future.
Do I need surgery? Am I going to have problems later in life? Can I still lift and get jacked? Will Dr. Dre ever release Detox?
I don’t know if we’ll ever hear Detox, but the answer to the other stuff is more promising.
I had a great follow-up question from my webinar on Flexion & Extension based back pain as part of The Complete Trainer’s Toolbox, and it gives us a great opportunity to discuss this and think critically about this topic:
“Do you consider exercises with reasonably high compressive and shear load to be risky for someone with disc herniations?”
Short Answer: No.
Long(er) Answer: It depends. We know that only Sith’s deal in absolutes – particularly on Tony’s site, because six other articles have made this gag. Lucky number seven for me.
Let’s break this question down into two smaller questions:
1) Are disc herniations always bad or problematic?
2) Will exercising under high levels of shear or compression increase the risk of pain, injury or further problems?
Are Disc Herniations Always Bad or Problematic?
No.
Many of us jump to the conclusion that when told we have a bulging or herniated disc, we’re doomed.
It’s normal to worry – our back hurts and we’re told there might be a problem with it that could threaten what we enjoy doing and how we earn money.
Whilst disc herniations can contribute to back pain, it doesn’t mean they absolutely will contribute to back pain.
One of the best things here is to look at research investigating the low back in pain-free populations. This study from 2015 pooled over three thousand pain-free people, and at least 30% of people had either a disc bulge or protrusion with no pain.
Nada.
Zilch.
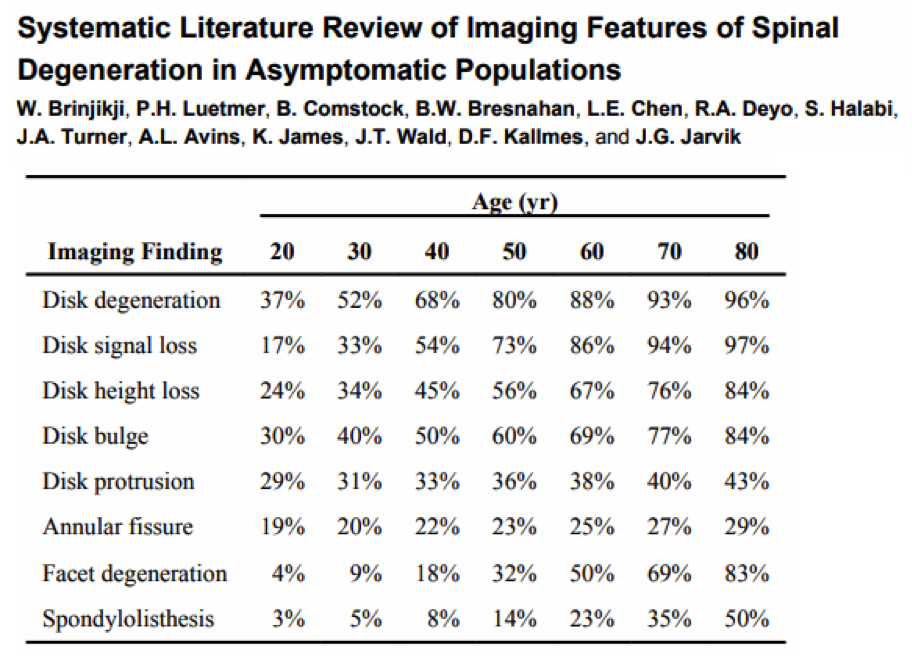
The other biggie here is a steady increase in pain-free findings as we age.
The older we get – the more likely it is to find ‘stuff’ on MRI, that doesn’t have to be a straight up cause of a client’s back pain.
So again, no, disc herniations are not a death sentence for your quest for jacktitude.
But
Pathology can still contribute to pain.
This research is great, but sometimes the pendulum swings a little too far, and these findings can be dismissed without proper assessment. Want to piss off your client who believes their back is due to a disc problem? Tell them outright it’s not a problem with no real justification other than ‘the research says MRI findings don’t matter’.
Rapport = gone.
But how do we know when to take notice of an MRI report or not?
Consider the concept of an active wound or healed scar to weigh up how relevant pathology is to pain. I picked these terms up from Dr. Stuart McGill, who knows a thing or two about spines.

He also knows a thing or two about awesome mustaches.
An active wound is where symptoms, assessment findings, and imaging reports all match up enough to connect the dots.
A healed scar is the presence of pathology on imaging, but without clear correlation to assessment findings. The dots are there, but not clearly connected at this point time.
Remember that an MRI is a single snapshot in time of your client laying on their back, doing nothing. It might look ‘bad’, but they might also be in no pain and crushing their training without fear or worrying about it.
How do you figure out whether you’re dealing with a wound or a scar?
Work with a healthcare professional who knows how to lift and help come to a clear understanding of your client’s back pain. Trainers are one million percent qualified to work with clients with back pain and disc herniations, when they have been screened and assessed properly.
Will Exercising Under High Levels of Shear or Compression Increase the Risk of Pain, Injury or Further Problems?
Short Answer: No.
Longer Answer: You need to ‘dose’ things appropriately.
As a quick refresher, spinal compression is the force that approximates each vertebrae. Spinal shear is the force that tries to pull one vertebrae forwards or backwards on another (at least in the sagittal plane).

Compression (image via Stronger by Science)

Shear (image via Stronger by Science)
The spine is designed to bear load, and the interactions of motions, loads and postures will load the spine in different ways.
What counts as ‘high’ levels of shear and compression?
If you’re a Sith dealing in absolutes:
- High shear loads come from a more horizontal torso angle and increased spine flexion
- High compressive loads come from greater loads lifted, more intense bracing strategies and a more extended spine position
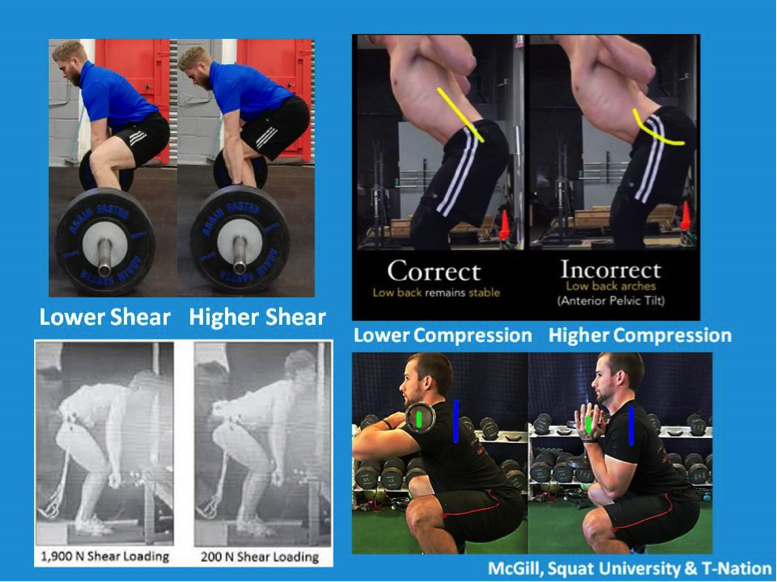
If you’re a Jedi and want to consider context:
- ‘High’ for a super heavy powerlifter will be different to ‘high’ for a yoga instructor
- ‘High’ for your client who has never lifted a weight is different to ‘high’ for your seasoned lifter who has accumulated decades of time under the bar.
- ‘High’ for someone in pain is different to ‘high’ for someone who is pain-free.
- ‘High’ is the upper end of an individual’s tipping point to tolerate load at that moment in time
This is where the science & art of training and rehab meet.
Science tells us that a conventional deadlift and back squat can probably allow us to lift the most load, but knowing your client would benefit more from front squats and trap bar deadlifts whilst their back hurts or if they are learning the ropes of lifting, is the art.

Don’t be this guy.
So what happens if we apply the appropriate ‘high’ level of stress with a disc herniation?
Just like everything else – discs will adapt
The body is a wonderfully adaptive organism that will react to the stresses placed upon it. If you get the dose of ‘high’ in the right ball-park, you will create positive adaptation. We’ve known about this the 80’s, where this study found the intervertebral disc positively adapts compressive load, yet it’s often viewed as a fragile structure that, when injured, spells game over.
Seems not.
This can be incredibly empowering for the clients suffering from back pain, whether it’s a diagnosed disc pathology or otherwise, that things can get better. This case study showed a huge improvement in a patient with an L4/5 herniation in just 5 months:
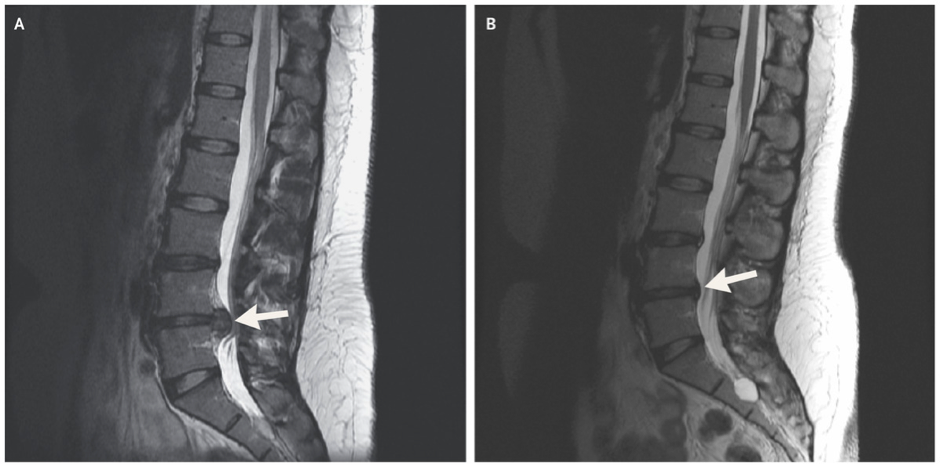
Credit – New England Journal of Medicine
Not sure if this applies to lifters?
Check out Brian Carroll’s MRI before and after working with Stuart McGill.
He started being disabled by pain with a broken sacrum and pretty banged up lumbar spine, but returned to the Powerlifting platform to set new world records at a lower bodyweight.

Credit – Brian Carroll
For me – this is where we need load within a low back rehab program.
If back pain stops us exercising, we will lose some level of fitness and adaptation as a result, which means we need to find a way back to exercising, based on what we can currently manage. I think this is why a lot of rehab programs don’t do well – it’s either too much load too soon which lead to flare ups and setbacks, or not enough load over time which means symptoms linger for longer than necessary.
So if we can say with confidence that disc herniations are not permanent, can get better and need load to return to our meaningful activities, how do we decide how to push it, when to push it, and how far?
Let’s answer these too.
How Do We Push It?
If you’re working with someone with back pain (or any pain really), your assessment should tell you this by answering this question;
“How much load can this client currently tolerate right now, and how can I best safely apply this?”
Don’t be afraid to use load in your assessments.
In fact, USE LOAD IN YOUR ASSESSMENTS.
A table and movement assessment is the starting point to see what the foundation is like, but how does what you see ‘at rest’ compare to when you’re at working weights?
Your client might have a perfect air squat, but if it resembles a melting handle at their working weight, you probably want to find that point where it looks good enough. Not perfect, not scratch-my-eyes-out terrible, just good enough.

Your 3/3 on the Overhead Squat won’t save you if you look like this under load.
If you start running into pain or problems under load, be comfortable enough to tweak the load, change the exercise variation, or coach it further. It’s OK if your assessment starts to resemble a training session, because it will give you way more information for your initial program with that client than relying on unloaded tests alone.
This is where you need the nuts and bolts of exercise progressions/regressions, coaching cues, and loading/tempo schemes to find the sweet spot for your client at that moment in time.
When Do We Push It?
Adaptation takes time, but it shouldn’t take forever. Your assessment gives you your starting point and how you feel during and after your lifting should guide how you progress. You don’t have to be pain-free, but you shouldn’t be pushing yourself through agony either. Here’s how I tend to work;
- Pain settled within 2 days and below a 3-4/10? Carry on wayward son.
- Pain longer than 2 days and/or above 5/10? Slow your roll.
Previous injury, pain, surgery or a lot of concern from your client will influence how quickly you choose to reapply the ‘stress’.
It’s ok to give it a little longer if needed, so know you can be flexible.
If things do go beyond what’s deemed acceptable, it doesn’t put us back to square one, but it might just require a little course-correction from time to time. No return from pain or injury ever moves in a nice linear, expected direction.

Credit – Sports Physio
As long as the loads, intensity and your client’s confidence and pain are steadily improving over time, you’re on the right track. Where ‘how’ is the science, ‘when’ is the art – know when to hit the gas, and when to pump the brakes, because it’s rarely a straightforward process.
How Far Do We Need to Push It?
What’s your client’s endgame?
The greater the demand of what your client is asking their body to deal with, the more time you’ll probably need. The new parent with a month or two of back pain wanting to pick up their kids without hurting and get 2-3 workouts in a week, will have a vastly different course to the powerlifter who’s been beaten up for years and wants to be out of pain and setting new world records.
Not everyone needs to hit soul-crushing, nose-bleeding levels of intensity, but if a client wants to work on their true maximum strength, you better be ready to take them back to working to 90% and above.
The goal of any rehab plan should be to build both physical and mental robustness that allows us to remain resilient to the stresses we want to place on ourselves, and still have enough in the tank to deal with the stresses we have to put on ourselves. As much as we want ourselves and our clients to crush their training sessions, it shouldn’t come at the expense of living the rest of their life the way they want to.
Remember – Disc Diagnoses Aren’t Death Sentences
The biggest challenge when someone is in the depths of an episode of back pain that may or may not have involved the ‘D’ word, is that they have the opportunity to get better and it’s not game over.
If we can get past this barrier, it becomes a matter of ‘when’ will they get better, not ‘if’. The intricacies of getting can be incredibly individual, but with the right approach, there’s no reason why you and your clients can’t get back to crushing it.
If you want to take a deeper dive on this – check out the Complete Trainer’s Toolbox, where I spend nearly three hours talking through what influences spinal loading during exercise, and how to plan a way back to beast-mode if back pain is a problem.
Ps – disc’s don’t ‘slip’ (courtesy of The Honest Physio).
About the Author
Alex works as a Physiotherapist in Essex, United Kingdom, with a special interest in working with those involved in strength and barbell sports.
Alex holds a triple bodyweight deadlift, and regularly publishes content through Rehab to Robust on Facebook & Instagram.






 Nicholas M. Licameli
Nicholas M. Licameli




 Tim is an exercise science graduate and CSCS who has been training in Baltimore MD for over 14 years. While his specialty is body composition, he has extensive experience working with clients from young athletes to cardiac rehabilitation patients. Tim has been published in a variety of fitness publications and writes for his blog when he isn’t helping clients in person.
Tim is an exercise science graduate and CSCS who has been training in Baltimore MD for over 14 years. While his specialty is body composition, he has extensive experience working with clients from young athletes to cardiac rehabilitation patients. Tim has been published in a variety of fitness publications and writes for his blog when he isn’t helping clients in person.




 Dr. Michael Infantino is a physical therapist. He works with active military members in the DMV region. You can find more articles by Michael at
Dr. Michael Infantino is a physical therapist. He works with active military members in the DMV region. You can find more articles by Michael at 

 Nicholas M. Licameli
Nicholas M. Licameli

