I’m currently with my family taking a little vacation down in Florida.1 I’ll be checking in at some point this week with some content, but on the meantime I’ve got some awesome people pinch-writing for me this week.
Today’s post is written by physical therapist Dr. Michael Infantino on a topic that’s a pain in the ass foot for a lot of people: plantar fasciitis.
Enjoy.

The 411 On Plantar Fasciitis & How to Make It Vanish
Lets set the scene: It’s a little after 5:00 am. As you open your eyes the sun is just starting to peak through your window. To your right, your husband; to your left, the band Maroon 5 casually playing an old hit. “Sunday morning rain is falling, steal some covers share some skin….”.
Just kidding it’s Sunday morning, rain is falling and you are dead set on getting that five-mile run in.
As you take the first step out of bed, the pain in your heel makes you rethink this whole running idea.
Unknowingly to your heel, your mind knows your day is going to drag if you don’t accomplish this feat.
I know the “drive” that runners possess.
The word “drive” and addictive personality disorder can sometimes be inter-changed, but that’s neither here nor there. This post is going to give you the 411 on everything plantar fasciitis is in as concise of a fashion as possible.
To make life easier we will just say heel pain.
Quick Rundown Of Todays Topics:
- WHO is more susceptible to developing plantar fasciitis?
- WHAT is plantar fasciitis? [Sounds like a skin eating disease.]
- WHAT can I do to treat this damn pain? [I know, I put “WHAT” twice. I wasn’t an English Major.]
- WHY am I not seeing progress?
WHO Is More Susceptible To Plantar Fasciitis?
Straight from the Journal of Orthopaedic & Sports Physical Therapy Guidelines for Plantar Fasciitis.
-
Overweight & Un-Athletic
I know, I know. This sounds awful. No one wants to be called overweight. More than that they don’t want to believe they fall into the un-athletic category.
Prime example: My dad (I love you dad). He has gained some lbs. over the years, and I wouldn’t classify him as an athlete by any means at this stage in his life. Despite my opinion, he still thinks he is SUPER.
His workouts usually come few and far in between. To my surprise, he can never quite understand why his body hurts after his impromptu 3-mile sprint (he calls it a jog) once every 3 months.
-
Runners
Yay runners! You made it into the JOSPT Guidelines. Victory! Wear this as a badge of honor… I think?
-
Workers That Spend Increased Time On Their Feet (i.e. factory workers)
-
Fearful Avoiders
No one wants to admit this characteristic. Regardless, it exists. Many people who actually develop chronic pain fall into this category. Your worries about causing more “damage” to your body often make you think bed rest is still a reasonable option.
I am sorry to say that it is not.
Runners, don’t smirk. You fall into the “overboard” category where your “driven” personality encourages you to push through pain. Because it is weakness leaving the body! Sometimes… not always.
The big takeaway here is to accept the fact that your job, your hobby or your current weight just makes this injury more likely. Knowing that this injury comes with the territory allows you to switch your focus to PREVENTION.
Give Me The Low Down On Plantar Fasciitis.
Research has continuously stated that your heel pain isn’t typically an “iitis,” or inflammation.
Ultrasound actually reveals increased thickening of the fascia near the insertion on the heel (Fabrikant, 2011). This sort of debunks the old “RICE” concept when trying to manage this injury.
It is safer to say plantar fasciopathy.
This could mean either an inflammatory or a degenerative process. Degenerative sounds scary. It isn’t. Changes in tissue quality are normal, not everyone has pain with these changes. [This one’s for you Fear Avoiders].
Diagnosing TRUE Plantar Fasciitis, Or “Fasciopathy.”
- 1st step in the morning reproduces heel pain
- Tenderness to touch at the insertion of the fascia on the heel
“Both were positive! Am I sentenced to months of night splints, orthotics and stretching?”
Not necessarily. If it is a true plantar fasciitis the research shows that these things can help. They may diminish symptoms, but it’s a Band-Aid.

JOSPT Guidelines
We need to be careful here. Some studies also showed that increased arch height was a predictive factor for pain. Your best bet is to have someone perform a running analysis to see what your foot is doing during the loading phase of running (preferably someone with a ton of knowledge about the human body).
If you don’t display “excessive pronation” or actually lack adequate pronation, an orthotic may not be a good fit. Excessive supination (opposite of pronation) while the foot is in contact with the ground during running or walking could actually be exaggerated with an orthotic.
Leading to ankle sprains.
JOSPT Guidelines
In my experience, night splints are hit or miss. With a true plantar fasciitis it could be a big hit. As I mentioned earlier, it is not actually fixing the source of the problem (the way you move, strength deficits, poor pacing etc). Before you sentence yourself to months of night splinting try to push the RESET button first.
Lets Get Started! Address Limitations In Ankle Mobility First.
1. Trigger Points
Work out those nasty tender points in your calves and the bottom of your feet. Calf trigger points can cause referral pain to the heel and bottom of the foot. Mimicking plantar fasciitis. Trigger points are responsible for reduced mobility, strength and timing of muscles! (Lucas, 2004)
BONUS: Self Instrument Assisted Soft Tissue Treatment (better than the roller stick… in my opinion.)
This is more of a soft tissue mobilization than trigger point treatment. It can actually be a great lead in to trigger point treatment. It helps reduce tone in the muscles. It is also a quick way to scan for areas that are more “stiff” and more irritated (increased trigger points local to that tissue). This is why I prefer it to the roller stick.
2. Stretch The Calves and Foot Musculature
Stretching feels good and it can help restore motion. BUT do not neglect the importance of strength and endurance at the shin musculature when looking to maintain that new length.
Performing strengthening drills, like the Shuffle Walk (courtesy of The Gait Guys) demonstrated in the video below will prevent increased tone in the calves from returning.
Prescription:
To make this more effective, actively pull the forefoot and toes up as you are stretching.
Pull the toes and forefoot up for 10 seconds (keep the heel down) followed by a 30 second stretch (work into it slow to get the desired effect). Repeat for 3 minutes.
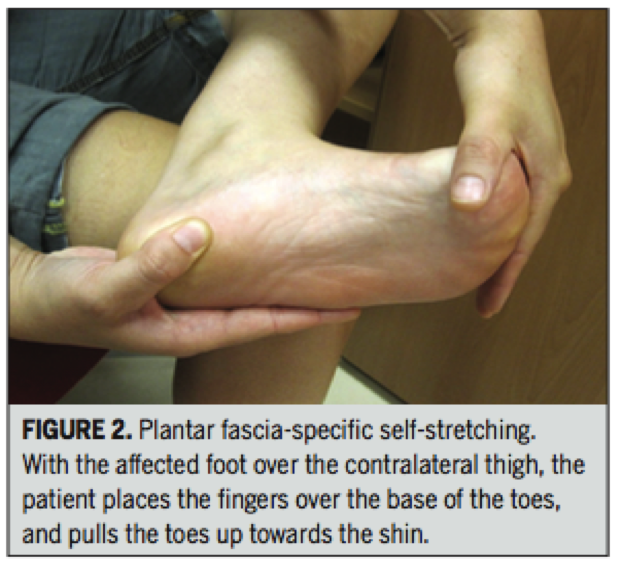
Renan-Ordine R, 2011
3. Attack The Joints
Get the joints in your ankles and feet moving more freely. Don’t forget about motion at that BIG TOE. Without proper extension at the big toe you can forget about actually accessing that new ankle motion.
This means you can’t access that hip extension while running. This equals poor gluteal function. It all goes down hill after that…
- 1st Toe Mobilization + Shuffle Walks
- Banded Ankle Mobilization With Active Dorsiflexion
This one is all over the Internet. From personal experience, having someone mobilize the ankle for you ends up being way more effective. But better than nothing!
- Self Ankle Manipulation
Great way to get some quick improvements. Combine with the other techniques!
Gave It A Go For A Couple Weeks And Still No Change?
The loss of considerable amounts of body fat obviously doesn’t occur overnight. Stick with a guided nutrition plan and exercise routine to work on weight loss without further aggravating any painful regions. This may require modifications in exercise choices for the time being.
If You Are An Avid Runner Or Stand A Lot For Your Job Consider The Following:
- Regular Shoe Rotation was found to be helpful in workers that spent more time on their feet. (Werner, 2010)
Your shoes really tell a story. Excessive pronation and supination start to wear down parts of the shoe. This exaggerates pronation and supination at the foot leading to increases in the speed at which these motions occur. Potentially leading to increased risk of injury.
- Orthotics/Taping
We discussed this earlier. Orthotics don’t always fix the problem, sometimes they can worsen it. Taping to support the foot or promote increase stability at the foot could be a safer and cheaper 1st step.
- Strengthening
The focus is typically on reducing “pronatory tendencies” at the foot. Sounds promiscuous, grrrrr! Tony can help you with that one.
Your ability to land in a good position during the loading phase of running, and continually do that over the course of a run is the primary goal; despite the addition of weight (maybe a ruck sack), speed or exertion.
Running is not an innate ability.
Strangely, I find joy in watching people run. It is easy to tell which people skipped some developmental milestones growing up or didn’t take part in too many athletic events. If you fall into one of those categories I would definitely recommend some training to improve your running mechanics.
- Leg Length Discrepancy (LLD)
I was hesitant to mention this because of how common LLD is in symptomatic and asymptomatic populations. However, it is mentioned in one study in the Plantar Fasciitis Guidelines (Mahmood, 2010). In various studies, a LLD of as little as 4-6 mm is considered clinically significant. In rehabilitation and the fitness world neuroscience is getting a lot attention; often disregarding biomechanics. It is probably in our best interest not to sweep this under the rug if we aren’t seeing progress. LLD will have an impact on your mechanics when walking and running.
Lets Wrap This Up!
The important thing to remember is that the recommendations made today are just guidelines based on an overwhelming amount of research. If you are in pain let these tips guide you. Don’t grasp on to them like they are the word of God, Buddha or The Dos Equis Guy. Accept the fact that your job, hobby, weight or lack of athletic ability make you more susceptible to this injury.
Fix the things you can, accept the things you can’t. There is no harm in trying out a cheap orthotic or heel pad for a little relief. If you want to take it a step further see a professional trained in running evaluations to determine needed changes in running mechanics, programming, proper shoe fit and/or orthotic fit. Knowledge is potential power. Go forth and conquer!
About the Author
Dr. Michael Infantino is a physical therapist who works with active military members in the DMV region. You can find more articles by Michael HERE.

References
Cotchett MP, Landorf KB, Munteanu SE. Effectiveness of dry needling and injections of myofascial trigger points associated with plantar heel pain: a systematic review. J Foot Ankle Res. 2010;3:18. http:// dx.doi.org/10.1186/1757-1146-3-18
Eftekharsadat, B., Babaei-Ghazani, A., & Zeinolabedinzadeh, V. (2016). Dry needling in patients with chronic heel pain due to plantar fasciitis: A single-blinded randomized clinical trial. Medical Journal Of The Islamic Republic Of Iran, 30401.
Fabrikant JM, Park TS. Plantar fasciitis (fasciosis) treatment outcome study: Plantar fascia thickness measured by ultrasound and correlated with patient self-reported improvement. Foot (Edinb) 2011;21:79–83. [PubMed]
Lemont H, Ammirati KM, Usen N. Plantar fasciitis: a degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc. 2003;93:234-237.
Lucas KR, Polus BI, Rich PS. Latent myofascial trigger points: their effects on muscle activation and movement efficiency. J Bodyw Mov Ther. 2004;8:160-166
Martin, R. L., Davenport, T. E., Reischl, S. F., McPoil, T. G., Matheson, J. W., Wukich, D. K., & McDonough, C. M. (2014). Heel pain-plantar fasciitis: revision 2014. The Journal Of Orthopaedic And Sports Physical Therapy, 44(11), A1-A33. doi:10.2519/jospt.2014.0303
Mahmood S, Huffman LK, Harris JG. Limb-length discrepancy as a cause of plantar fasciitis. J Am Podiatr Med Assoc. 2010;100:452-455. http:// dx.doi.org/10.7547/1000452
Renan-Ordine R, Alburquerque-Sendín F, de Souza DP, Cleland JA, Fernán- dez-de-las-Peñas C. Effectiveness of myofascial trigger point manual therapy combined with a self-stretching protocol for the management of plantar heel pain: a randomized controlled trial. J Orthop Sports Phys Ther. 2011;41:43-50. http://dx.doi.org/10.2519/jospt.2011.3504
Werner RA, Gell N, Hartigan A, Wiggerman N, Keyserling WM. Risk factors for plantar fasciitis among assembly plant workers. PM R. 2010;2:110-116. http://dx.doi.org/10.1016/j.pmrj.2009.11.012